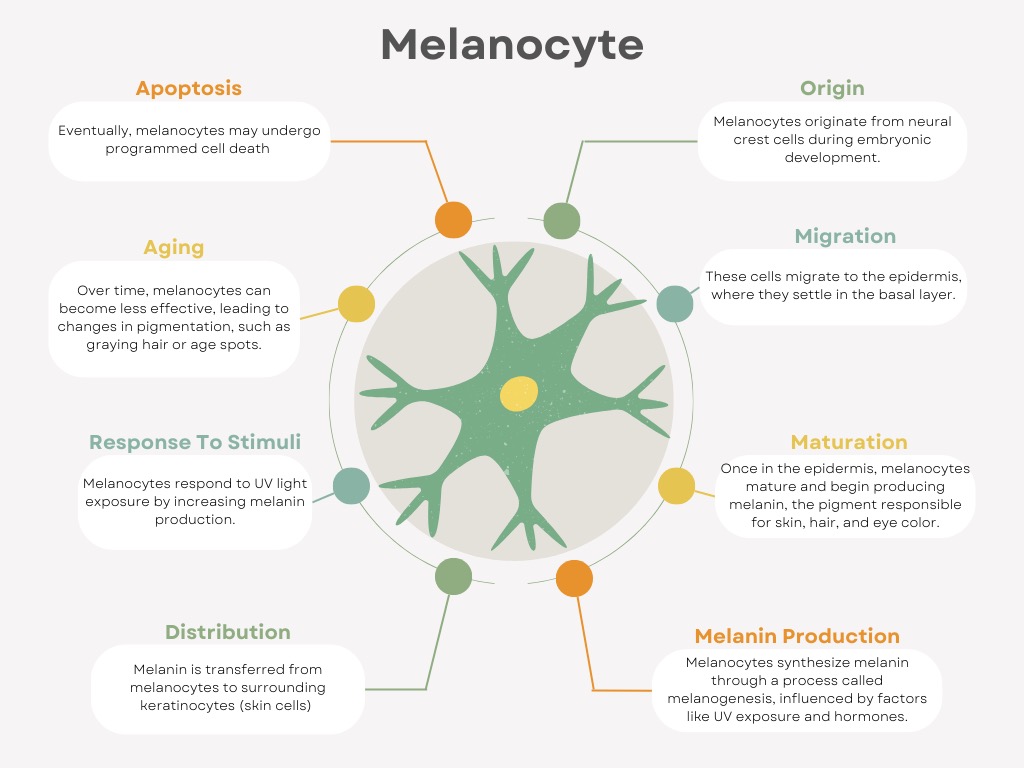
Recently Jenna Dewan, celebrity and judge on Come Dance With Me, opened up about her stubborn melasma and showed amazing results after treatment with lasers. While there are incredible treatments now available, it is important to remember that hyperpigmentation is a life-long condition that requires a whole team of products and providers. Let’s explore the life cycle of the melanocyte to start.
Hyperpigmentation, characterized by darkened patches of skin, is influenced by how the melanocytes (pigment-producing cells) function during their lifecycle. Several factors, including UV exposure, hormonal changes, and skin injury, can trigger an overproduction of melanin, resulting in hyperpigmentation. Understanding how home care, brightening ingredients, tyrosinase inhibitors, SPF, and various treatments like chemical peels, laser resurfacing, microdermabrasion, hydrodermabrasion, and dermaplaning affect melanocytes at each stage of their lifecycle can help manage hyperpigmentation more effectively.
Dr. Chantal Lunderville, L+A Medical + Wellness Editor
Dr. Chantal Lunderville is a board-certified physician specializing in skin health, aesthetic medicine, and Women’s health. She attended medical school at UCLA School of Medicine, followed by a residency at UCSF Family Medicine, and on graduating opened her own concierge aesthetics practice in the San Francisco Bay Area focusing on hormone health, skincare, and longevity.
Since then Dr. Lunderville has grown her practice to include overseeing nurses and aestheticians as medical director to over 15 practices across California, and through Dr. C’s Academy helps to launch new practices across the US and Canada through consulting and online courses in business, compliance, aesthetic procedures including neurotoxin, fillers, lasers, microneedling, and lasers. Read Full Bio
1. Origin and Home Care
Melanoblasts are precursor cells that eventually mature into melanocytes. Though hyperpigmentation concerns typically arise after melanocytes are fully functional, early skin care can influence how healthy and resilient the skin becomes through lowering inflammation and ensuing healthy melanocytes. We need to ensure our patients follow gentle cleansing, hydration, and protection from environmental stressors daily.
2. Melanoblast Migration and Brightening Ingredients
As melanoblasts migrate to the epidermis, the potential for future pigmentation issues can be addressed through brightening ingredients like vitamin C, licorice extract, and niacinamide. These ingredients help inhibit melanin overproduction and prevent the formation of dark spots before melanocytes become fully active. While melanoblasts are not yet producing melanin, ensuring that the skin environment is healthy can set the stage for balanced pigmentation later on.
3. Maturation and Tyrosinase Inhibitors
Once melanoblasts differentiate into melanocytes, they begin producing melanin in response to stimuli like UV radiation, hormones, genetics, and inflammation. Tyrosinase inhibitors—such as arbutin, Vitamin C, kojic acid, and hydroquinone—become crucial in managing hyperpigmentation at this stage. Tyrosinase is the enzyme responsible for melanin production. By inhibiting this enzyme, these ingredients reduce melanin synthesis, helping prevent dark spots and uneven pigmentation.
4. Melanin Production and SPF
At the height of melanin production, SPF becomes one of the most essential tools for preventing hyperpigmentation. Exposure to UV radiation triggers the melanocytes to produce more melanin as a protective response. We encourage mineral-based SPF 80 or above, reapplication, as well as hats, protective clothing, and finding shaded areas. Patient education is key as well as easy reapplication products.
5. Regulation of Pigmentation and Chemical Peels
Once melanocytes are actively producing melanin, the skin may develop uneven pigmentation, especially in response to factors like sun exposure or hormonal changes. Chemical peels (e.g., glycolic acid, lactic acid, TCA, AHAs) are highly effective at addressing hyperpigmentation during this phase. By exfoliating the outer layer of skin, peels accelerate cell turnover and remove pigmented cells, revealing fresher, more even-toned skin underneath. Retinoids also assist with this, by encouraging cell turnover.
6. Aging and Decline: Laser Resurfacing, Microdermabrasion, Hydrodermabrasion, Dermaplaning
As melanocytes age and their function declines, hyperpigmentation often becomes more visible due to accumulated sun damage, decreased melanin regulation, or hormonal factors. Several treatments can target these issues:
- Laser resurfacing uses targeted light energy to break up areas of pigmentation and stimulate new skin growth. Examples include IPL, Clear & Brilliant, Coolase (deeper pigment such as melasma) or Smartlase CO2 (superficial pigment). This method is especially effective for deep or stubborn pigmentation, as it can penetrate the skin more deeply than other treatments*. See in action here
- Microdermabrasion is a non-invasive exfoliating treatment that removes the outermost layer of skin, which helps lighten superficial pigmentation and improve skin texture.
- Hydrodermabrasion combines exfoliation with hydration, helping to remove dead skin cells while infusing the skin with hydrating and brightening ingredients. This is gentler than traditional microdermabrasion but still effective at managing hyperpigmentation.
- Dermaplaning is a manual exfoliation technique that removes dead skin and peach fuzz, allowing products like tyrosinase inhibitors and brightening agents to penetrate deeper into the skin. This treatment can help reduce surface pigmentation and make the skin more receptive to other treatments.
7. Cell Death or Senescence: Long-term Care
As melanocytes enter senescence (cell death or aging), pigmentation concerns often become less about the overproduction of melanin and more about uneven skin tone, including age spots. Even without a focal spot or melasma, patients will experience brighter more even skin tone with these treatments, contributing to their anti-aging goals and satisfaction.
Timing of Treatments
My #1 recommendation for treating stubborn pigment for patients is to set expectations with patients and create a long-term plan that includes their daily home care and in-office treatments. We can most effectively target pigment by delivering a heavy treatment upfront such as a short course, ie maximum of 4 weeks, of Triluma (fluocinolone acetonide 0.01% (0.1 mg), hydroquinone 4% (40 mg), and tretinoin 0.05% (0.5 mg) followed by maintenance with daily ingredients such as niacinamide, kojic acid, with intermittent facials or chemical peels, and a series of lasers yearly. There is some role of diet and oral vitamins to play as well in cell turnover, for more on this check out Des Fernandes’s book here.
In conclusion, melanin is stubborn but if we can understand the physiology then we have an advantage in creating a customized plan for each patient. As you can see, it requires everyone from the aesthetic team to a well-timed long-term treatment plan and patient education. Let us know your thoughts in the comments below!
*IMPORTANT: Lasers can worsen hyperpigmentation if done improperly or due to improper patient selection. For further information on training please contact us at Élev Institute for further support for your spa.